The blood is milky white, the man has to change the plasma urgently in the night
A 40-year-old male patient was admitted to a hospital in Phu Tho with severe epigastric pain, abdominal distension, abdominal CT scan results showed that the patient had acute pancreatitis, bathazal D, and blood triglycerides were elevated (55 mmol). /L while the average person is 0-2.3 mmol/L).
In particular, the blood taken out is milky white. Immediately, the patient was assigned an emergency plasma exchange in the night.
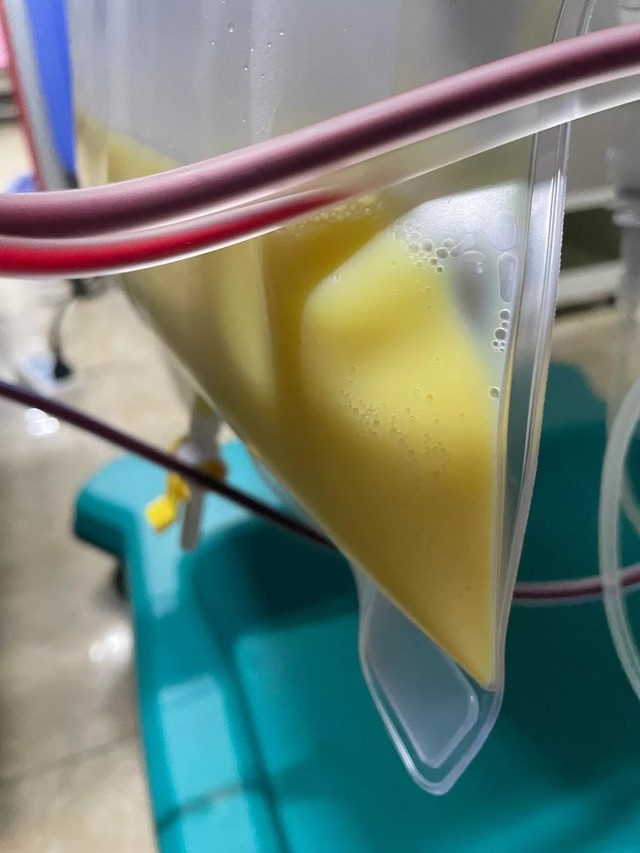

The blood taken out was as white as milk, and the patient was immediately assigned an emergency plasma exchange in the night. Photo: BVCC
After plasma exchange, the patient had a positive change, no more abdominal pain. Decreased triglycerides in the blood.
BS. Luong Minh Tuan said, plasma replacement therapy is to take out a large amount of plasma (usually 1-1.5 times the patient’s plasma volume), then replace with an appropriate amount of the same volume. accumulate.
Blood cells that are separated from the plasma are returned with the replacement fluid into the body to maintain intravascular volume. Substitutes for the patient’s plasma can be 4%-5% albumin or fresh frozen plasma (FFP).
Cases of acute pancreatitis due to hypertriglyceridemia usually respond very well to this treatment.
According to TS.BS Duong Minh Thang, Digestive Emergency Department – 108 Hospital, acute pancreatitis is an acute inflammatory disease of the pancreas, characterized by the frequent development of local and systemic complications. This is a common problem in the emergency department of hospitals.
1. Causes of acute pancreatitis
Dr. Thang said that up to 40-50% of the causes are biliary diseases caused by stones or worms.
Alcohol is also very common (accounting for 20 – 30%). Typically, the above patient has a history of heavy drinking, cirrhosis, hepatitis C virus.
In addition, less common causes may be abdominal trauma or surgery, endoscopic retrograde cholangiopancreatography (ERCP); Diseases causing damage to small blood vessels such as diabetes, lupus erythematosus; Diseases with hyperlipidemia such as nephrotic syndrome or a group of disorders of blood lipid metabolism.
Hypercalcemic metabolic disorders such as hyperparathyroidism; viral infections (mumps, CMV, EBV); due to drugs; Allergies… are also the causes of acute pancreatitis, although rare. However, in about 20-25% of cases the cause cannot be determined.
2. Clinical symptoms of acute pancreatitis
According to Dr. Thang, a clinical symptom of acute pancreatitis, of which the first is abdominal pain. The cause is due to the patient’s pancreatitis, retroperitoneal drainage or peritonitis. The pain often starts suddenly, after a full, fatty meal, after a party. Pain is often acute and severe in nature. Patients often have pain in the upper umbilicus, left side, spreading to the left back.
Patients may experience nausea and vomiting with the following characteristics: Vomiting profusely and continuously; After vomiting does not relieve pain.
In addition, the patient may have other symptoms:
Fever, if present early in the first 2-3 days. Jaundice if mild, subtle jaundice is usually due to edema of the common duct. If jaundice is obvious, it is usually due to biliary disease associated with stones or worms. Intestinal disturbances often include paralytic ileus and abdominal distension. Abdominal effusion is common in severe cases, sometimes with bloody ascites. Left pleural effusion is less common and also has a severe prognosis.
Doctors said that the symptoms of acute pancreatitis were rampant, complicated, and fast. Even when the crisis is over, complications of infection, poisoning, and exhaustion are still lurking. The disease is easy to relapse many times. Therefore, patients always need to be closely monitored medically and strictly follow the treatment instructions of the doctor.
3. Complications of acute pancreatitis
– Shock if occurring early in the disease, usually due to hemorrhagic complications or toxicity with kinins. If due to infection, shock usually occurs later in the 2nd week of illness.
– Bleeding in the pancreas, in the abdominal cavity, in the gastrointestinal tract or in distant organs due to pancreatic enzymes damage blood vessels, severe prognosis.
– Infection in the pancreas usually occurs at the end of the first week or the beginning of the 2nd week of the disease, leading to the establishment of pancreatic abscess and necrotic tissue, with a severe prognosis.
– Acute respiratory failure (ARDS): The prognosis is severe.
– Pancreatic pseudocyst usually appears in the 4th week of the disease due to the encapsulation phenomenon to localize the lesion. Pancreatic pseudocysts can be absorbed or drain on their own into the pancreatic duct and resolve in 4-6 weeks. Cysts can also persist longer and can lead to complications such as superinfection and abscess.
– Chronic pancreatitis due to recurrent acute pancreatitis, mostly acute pancreatitis in alcoholics. Therefore, in alcoholics, it must be noted that there may be an acute episode of chronic pancreatitis.
at Blogtuan.info – Source: cafebiz.vn – Read the original article here



